Rural Colorado hospitals, health centers expect $1B in federal investments over next 5 years
The money, which is far more than what state officials had been anticipating to get, will come from congressional Republicans’ One Big Beautiful Bill Act
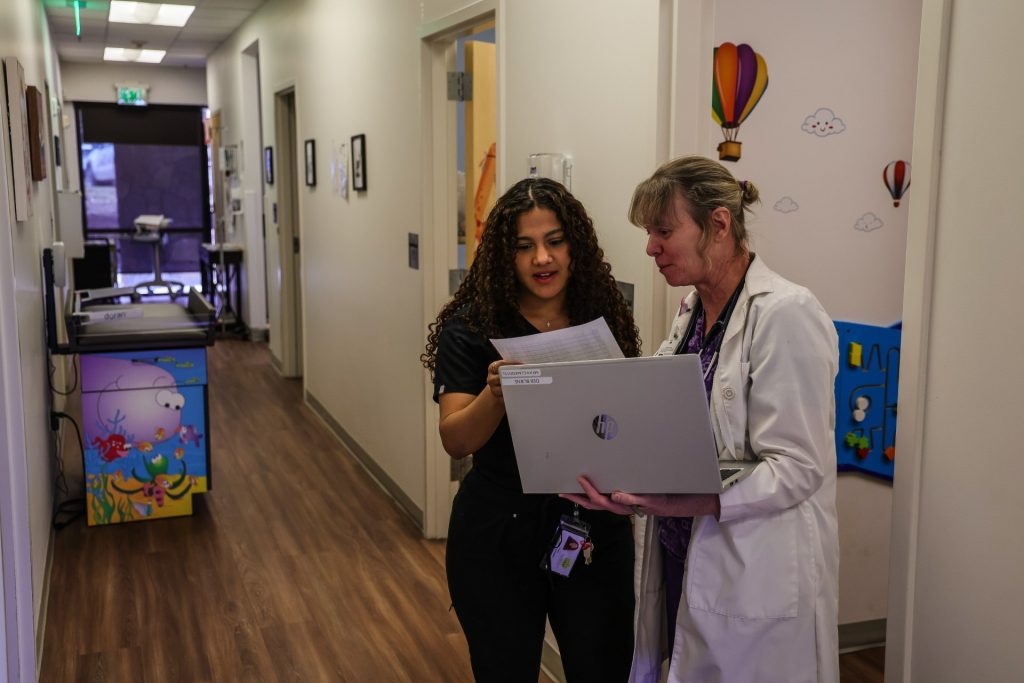
Chris Dillmann/Vail Daily
Colorado is expected to receive $1 billion in new federal funding for rural health care over the next five years, far more than what officials had initially anticipated when they applied for the money this fall.
The funding comes from President Trump’s “big beautiful bill” that was passed by the vast majority of congressional Republicans and signed into law by Trump over the summer.
The sweeping domestic policy bill includes $50 billion to support rural health programs in all 50 states. The provision was added later into the bill’s crafting, partly in response to concerns about how the legislation’s Medicaid cuts would affect rural hospitals and health centers.
The Colorado Department of Health Care Policy and Financing, which oversees the state’s Medicaid program, said on Dec. 29 it had been approved for just over $200 million in first-year funding. In total, the state expects to see over $1 billion in funds through 2030.
“Our rural health care providers help break down barriers to critical care for Coloradans across our state,” said Gov. Jared Polis, in a statement. “This new funding will help us strengthen our rural health care system by supporting providers and increasing access to care for everyone in our rural communities.”
The funding amount surpassed the expectations of state officials, who had hoped to receive at least $100 million each year — or approximately $500 million over the federal program’s lifetime.
“We shouldn’t rely on or assume that we’ll get $1 billion,” said Colorado Department of Health Care Policy and Financing CEO Kim Bimestefer, during a virtual webinar in early December.
States had to move at a swift pace to apply for the funding, with applications formalized in mid-September and due Nov. 5. Bimestefer described the application as “complicated” with “very specific guidelines” that put states in competition with one another.
While half of the $50 billion is set to be distributed equally among all states, the remaining funds will be allocated based on factors such as rural population size, the number of rural health centers, and the level of uncompensated care. States also had to outline plans for how they would use the funding to improve rural health systems and ensure they would align with federal health policies, such as the Trump administration’s Make America Healthy Again agenda.
Bimestefer, in a statement on Dec. 29, said the investments will drive “game-changing improvements across rural care access, innovation, affordability and health outcomes across rural Colorado for generations to come.”
What the funding will cover, and what it won’t
Colorado health officials said the federal funds will serve all 52 of the state’s rural and frontier hospitals located on the Western Slope and the Eastern Plains. Those account for approximately 13% of the state’s health care facilities across all provider types.
Officials plan to use the funding to help support rural counties with the highest rates of chronic diseases or preventable hospitalizations, as well as frontier counties that lack critical specialty care access, including behavioral health, obstetric, and gynecology services.
“Rural facilities serve over 800,000 people living in Colorado’s 52 rural counties,” said Colorado Rural Health Center CEO Michelle Mills, in a statement. “We are grateful for this rural transformation funding as it will provide the opportunity to keep essential services local and develop new creative solutions through workforce, technology, and innovation.”

Along with hospitals, the funds will be used to support federally qualified health centers (also known as community clinics), behavioral health providers, opioid treatment programs and emergency medical services. State officials also plan to direct some funding to Colorado’s two federally-recognized tribal nations: the Ute Mountain Ute Tribe and the Southern Ute Indian Tribe.
What that support looks like in practice may vary widely. It could include training and continuing education opportunities for rural providers; increasing regional collaboration through shared electronic medical record systems; updating health centers’ technology and IT support; paying for credentialing, certifications and application fees for rural residents seeking to become health care workers; and expanding telehealth services.
Still, states are limited in how they can deploy the funds.
States cannot, for example, use the money to duplicate existing programs already covered by federal funds. Funding also cannot be used to cover construction costs for health centers, and no more than 15% of a state’s total funding can be used to cover provider payments.
Mills, during the webinar hosted by health officials earlier this month, said those provisions came as a “disappointment.” She said that “a lot of people that we heard from really wanted a lot of the money to go to provider payments,” and that the state has “a lot of aging (facilities) that were built in the (1950s and ’60s) that are needing replacement, and those funds are hard to find.”
Other health care cuts still loom

While state health officials celebrated the money as a needed boost for rural Colorado, they’ll still have to contend with large federal funding cuts for other programs over the coming years.
Included in congressional Republicans’ “big beautiful bill” are measures that will reduce the scope of Medicaid by instituting new work and renewal requirements for beneficiaries as well as limiting access for some immigrant populations.
The law also reduces the federal government’s share of Medicaid funding for states by limiting what is known as provider taxes, or fees, which states levy on hospitals to draw down more federal Medicaid dollars.
Most of those changes start in 2027.

In total, the provisions are expected to cut Medicaid spending by $1 trillion nationally over the next decade, according to projections by the Congressional Budget Office, the nonpartisan body that reviews the fiscal impacts of federal policy.
Colorado stands to lose billions of dollars over the coming years as a result. The reduction in provider fees alone could cost the state’s hospitals $10.4 billion by 2032, according to the Colorado Hospital Association.
Mills said earlier this month that while the funding will be important for rural communities, “This in no way is going to cover the Medicaid cuts” included in the “big beautiful bill.”
Colorado’s health systems could face further pressure due to the expiration of federal subsidies for Affordable Care Act insurance plans, which lapse on Jan. 1. The loss of subsidies is poised to send insurance premiums surging for potentially hundreds of thousands of Coloradans who purchase their insurance on the state’s individual marketplace.
Rural enrollees face some of the biggest cost increases, with some mountain town residents reportedly facing premium increases in 2026 as high as 400%. Some have considered changing to a lower premium plan that will come with higher deductibles and fewer coverage options, while others may drop their insurance altogether.
Doing so could drive more uncompensated care to hospitals, many of which already struggle with low to negative profits, health care advocates have warned.

Support Local Journalism

Support Local Journalism
The Sky-Hi News strives to deliver powerful stories that spark emotion and focus on the place we live.
Over the past year, contributions from readers like you helped to fund some of our most important reporting, including coverage of the East Troublesome Fire.
If you value local journalism, consider making a contribution to our newsroom in support of the work we do.










